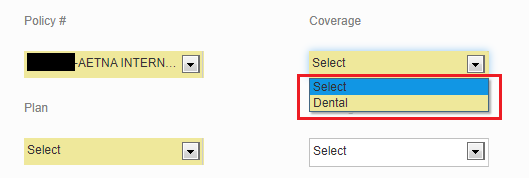
Plan Not Available in Coverage Dropdown
The plans shown in the online portal are based upon the member's home state address. If you're looking to add Medical coverage for a member but only Dental coverage is showing,
or if you're looking for a plan that is not listed,
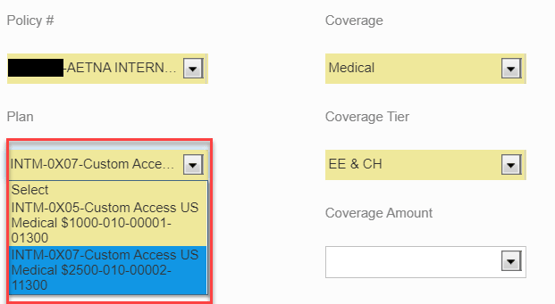
then there are two reasons why the plan might be unavailable:
- Aetna does not create plans for states until they are needed.
- If a group is headquartered domestically (Washington or Alaska), Aetna does not create the plan until there is a member that needs to enroll on it. For example, if the group offers the Gold 500 plan and the Silver 2500 plan and the member is enrolling on the COBRA Silver 2500 plan in the state of Idaho then Aetna will only create that specific plan.
- When a group is headquartered internationally, then Aetna does not create the plan until there is a member that needs to enroll in that state. For example, if the group offers the Gold 500 plan and Silver 2500 plan and the member is enrolling on the COBRA Silver 2500 plan in the state of Idaho Aetna will create all the plans available in Idaho.
- If the group is headquartered internationally and the plan is listed in the account structure but not listed in the online portal, it might not be loaded into TBS's system because no one is enrolled on it.
To have the plan the member needs to be enrolled on added to the portal, please reach out to our Client Care team and provide the following:
- Groups headquartered internationally: globalbilling@tbsmga.com
- Groups headquartered in WA: billing@tbsmga.com
- Groups headquartered in AK: billing.ak@tbsmga.com
If the group is headquartered domestically, please provide a completed enrollment application so our team can submit the site add request to Aetna for processing. Once the site add request has been submitted please allow 10 to 15 business days for processing. Once the site add is complete it will be available in the portal for all members going forward.
If the group is headquartered internationally, please provide sufficient information for our team to identify the member record along with any information that has not been entered into the online portal.
- If the plan is already part of the account structure, we will ensure it's loaded in the system where it will be available going forward and the member is enrolled on the plan.
- If the plan is not part of the account structure, we will submit the site add request to Aetna and enroll the member on the base plan until the site add request has been completed.
Related Articles
OBS Employee Maintenance Page
Enrolling an Employee (New Hire or Open Enrollment) Enrolling an Employee with a Qualifying Life Event Adding a Dependent Terminating an Employee Removing a Dependent Search Employee Navigate to the Employee Maintenance page. Select ...OBS Eligibility Change Restrictions
The following enrollment changes are not designed to be completed through the TBS Online Billing System and should be completed as outlined in each section below. COBRA/State Continuation Enrollments Please submit all COBRA or State Continuation ...OBS Reports Page
Employee Participation Report This report will generate a current census. The filters are customizable. The 3 required fields are highlighted in yellow. From the Reports tab, click on Employee Participation Summary Enter the required field, Carrier. ...